2022-05-26
The Rising Prevalence of Skin Cancer in Canada
Share:
MDBriefCase will be unavailable due to maintenance from Sunday, January 14 11PM to Monday, January 15 1AM ET.
Welcome
Skin cancer is the most common of all cancer types in Canada, accounting for an estimated one-third of new cancer cases diagnosed each year.
Skin cancer can be classified as melanoma and non-melanoma – non-melanoma skin cancer (NMSC) can also be further separated as basal cell carcinoma (BCC) and squamous cell carcinoma (SCC) based on the type of cell in which the cancer originates. Melanoma is a cancer that develops in the skin’s melanocytes, or the skin cells located near the bottom layer of the epidermis that produce melanin.
Most skin cancers detected in Canada are non-melanoma and typically occur on areas that receive frequent sun exposure, including the face, neck, and hands. Melanoma accounts for approximately 5 percent of skin cancer diagnoses and can develop almost anywhere on the body, even in areas that receive little to no sun.
As incident rates of both melanoma and non-melanoma skin cancers rise, so do mortality rates, with numbers increasing five-fold in some provinces in recent years.
It’s now estimated that 1 in 42 men and 1 in 56 women will develop melanoma during their lifetime, and 1 in 219 men and 1 in 402 women will die of it.
Early detection is key – when caught early, melanoma can be treated successfully with survival rates between 40-97 percent, however once metastasis occurs, survival rates drop substantially to 15-20 percent.
Family physicians are often the first line of defense in detecting skin cancer – ensuring you and your patients know what to look for can save lives.
Though there is no single cause of skin cancer, approximately 90 percent of skin cancers are caused by UV rays. Other factors that enhance risk include:
Checking your skin often for changes and new lumps, bumps or growths is critical to catching skin cancer early when it’s easier to treat. Though not all skin cancers will look like the examples below, the following are general guidelines on what to look for.
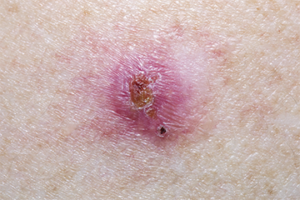
Most BCC initially appear as a small ‘pearly’ bump similar to a flesh-coloured mole or pimple that does not go away. Growths can also appear dark in colour, or as pink patches with scaling or a slightly shiny appearance. They can also appear as hard, scar-like growths.
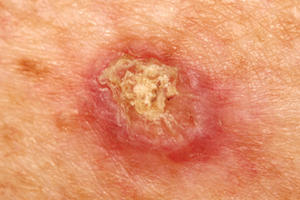
Most incidents of SCC are caused by sun exposure or sun damage. In early stages, SCC can appear as small, skin-coloured or red nodules, usually with a rough surface. They can also resemble warts or bruises with raised, crusty edges. Lesions develop slowly, but over time, can grow into a large tumor. Crusting, ulceration, and bleeding might occur.
The first sign of melanoma is typically a change in the shape, colour, size, or feel of an existing mole, however it may also appear as a new mole. Melanoma occurs most frequently on the legs for women, and on the chest or back for men, however they can be found on the face and neck and in areas not typically exposed to the sun.

The ABCDEs and the Ugly Duckling methods are both frequently used to detect melanoma.
When checking moles, look for:
Asymmetry. Most melanomas are asymmetrical – if you draw a line through the middle of the lesion, the two halves would not look the same.
Border. Melanoma borders tend to be uneven and may have scalloped or notched edges.
Colour.Normal moles are usually a single shade of brown. A melanoma may have multiple colours, including different shades of brown, tan or black. As it grows, white, red or blue may also develop.
Diameter. Look for lesions the size of a pencil eraser (6mm) and larger.
Evolving. Look for any changes in size, shape, colour or elevation of a spot on your skin, or any new symptoms such as bleeding, itching or crusting.
Ugly duckling lesions are moles or spots that look different from surrounding moles. They will typically appear larger, smaller, lighter, or darker than their neighbours.
The best way to lower your risk of developing skin cancer is to be sun smart.
+ + +
Clinicians: Stay current on the latest skin cancer diagnosis and treatments. This complimentary course from MDBriefCase will improve your ability to:
In submitting your work (the “Work”) for potential posting on the MDBriefCase Healthcare Leadership Academy website (the “Website”), you (“You”) expressly agree to the following:
Review: MDBriefCase is pleased to consider the publication of Your Work on the Website. The suitability of the Work for posting shall be determined by MDBRiefCase at its sole discretion. Nothing herein shall obligate MDBriefcase to post or otherwise publish the Work, or the maintain its posting in future.
Editing; Identification: MDBriefcase shall have the right to edit the Work to conform to our standards of style, technological requirements, language usage, grammar and punctuation, provided that the meaning of the Work is not materially altered. If posted, You will be identified as the author of the Work, or co-author if applicable.
Grant of Rights: As a condition of publication and for no monetary compensation, You hereby grant to MDBriefCase the following rights to the Work in any and all media whether now existing or hereafter developed, including print and electronic/digital formats: (1) the exclusive right of first publication worldwide; (2) the perpetual non-exclusive worldwide right to publish, reproduce, distribute, sell, adapt, perform, display, sublicense, and create derivative works, alone or in conjunction with other materials; (3) the perpetual non-exclusive worldwide right to use the Work, or any part thereof, in any other publication produced by MDBriefCase and/or on MDBriefCase’s website; and (4) the perpetual non-exclusive worldwide right to use the Work to promote and publicize MDBriefCase or its publications. The grant of rights survives termination or expiration of this Agreement.
Warranty: You warrant that the Work is original with You and that it is not subject to any third party copyright; that You have authority to grant the rights in this Agreement; that publication of the Work will not libel anyone or infringe on or invade the rights of others; that You have full power and authority to enter into this Agreement; that the Work has not been published elsewhere in whole or in part; and that You have obtained permission from the copyright owner consistent with this Agreement for any third party copyrighted material in the Work. This warranty survives termination or expiration of this Agreement.
Thank you for your interest in writing an article for the MDBriefCase Healthcare Leadership Academy website.
The Healthcare Leadership Academy welcomes submissions on all topics relevant to leaders in healthcare. Our topics include Leading in Healthcare, Leadership Lessons from COVID-19 and others. We prioritize stories that provide leadership advice to executives and managers in healthcare companies, offer actionable strategies for executing successful projects, and provide interesting angles on current healthcare topics. Submissions must be original work of the authors and unpublished. When submitting, authors represent that they have included no material that is in violation of the rights of any other person or entity.
Articles must be educational and non-promotional. If they mention the author’s company or any of the company’s products or services by name within the text, such mention should be very limited and used for reference only, not for promotion. (For example, an author might cite a survey conducted by his company but not describe his company’s product as a solution to a business problem.) Articles will be edited for clarity, style and brevity. The final headline is determined by the editor.
Guest articles for the MDBriefCase Healthcare Leadership Academy may run between 500 and 1000 words.
MDBriefCase reserves the right to accept or reject any submission and the right to condition acceptance upon revision of material to conform to its criteria.
There is no payment for contributed articles. However, MDBriefCase will give the author a byline. Authors are invited to link to the article on personal websites, corporate websites and social media platforms.
Each author understands and agrees that any submission accepted for posting is provided subject to MDBriefCase’s Author Agreement.
This website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognising you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.
Strictly Necessary Cookie should be enabled at all times so that we can save your preferences for cookie settings.
If you disable this cookie, we will not be able to save your preferences. This means that every time you visit this website you will need to enable or disable cookies again.
This website uses Google Analytics and other tools to collect anonymous information such as the number of visitors to the site, and the most popular pages. Additional information may be collected for analysis.
Keeping this cookie enabled helps us to improve our website.
Please enable Strictly Necessary Cookies first so that we can save your preferences!